What ails India’s massive diagnostics sector: putting labs under the lens
• Shankar Dhange, 27, has been fighting against the private diagnostics sector in Maharashtra for years.
• His sister, Sarika Bhonglat, died six years ago due to incorrect tests and incorrect treatment.
• The diagnostics sector in India is facing a shortage of trained personnel to meet the rapid growth of medical laboratories.
• The sector accounts for around 9% of the healthcare industry, estimated to be worth ₹860 billion in 2024 and projected to grow to ₹1,275 billion by 2028.
• The Clinical Establishments (Registration and Regulation) Act 2010 aims to bring all diagnostic centres and labs under its ambit, with their registration with respective State councils.
• India has a highly fragmented market with many small, unorganised labs, largely not accredited, and following uneven quality standards.
• The fast-paced growth of the private sector creates challenges such as low entry barriers and lack of a strong regulatory environment.
• N. Venkateswaran, CEO of NABL, highlighted the challenges created by the fast-paced growth of the private sector, including a highly fragmented market with many small, unorganised labs, uneven quality standards, and inadequately skilled manpower.
India’s Diagnostics Industry: Manpower Shortage and False Reports
• India’s diagnostics industry is facing a significant shortage of full-time doctors and staff, affecting the quality of outcomes.
• Accredited labs must mandate the hiring of a full-time lab technician/phlebotomist and a radiologist.
• Research by the Health Ministry indicates India lacks enough microbiologists and qualified doctors or technicians to operate a lab.
• There is a lack of upgrading and training, and geographical inequality in service quality.
• Lab reports often contain ‘bought out’ signatures from doctors, indicating the presence of “ghost employees and doctors.”
• The Karnataka Private Medical Establishments (KPME) Act governs healthcare facilities, but its enforcement in the labs and diagnostics sector is limited.
• Many hospitals and doctors run clinics have side laboratories and sample collection centres, which are not run or owned by qualified pathologists.
• The issue affects patients, with cases of identity theft and fraudulent practices by lab technicians.
• The Maharashtra Paramedical Council Act, 2011, and the National Commission for Allied and Healthcare Professions (NCAHP) Act 2021 do not permit laboratory technicians to practice independently and issue reports without certification by a pathologist.
India’s Diagnostics Sector Challenges and Solutions
Urban-Rural Divide
• Only 24% of diagnostics revenue comes from rural areas in India, despite 70% of the population living in rural areas.
• Government-private labs divide exists due to gaps in standards and staff shortages.
• In Telangana, government hospitals require upgrades and limited operational hours, causing patients to seek private care.
Pricing Problem
• Pricing is a concern in the private health sector, with some government programs and states addressing this issue.
• The Telangana Diagnostics Programme (T-Diagnostics) initiative in Telangana conducted over 18.10 crore tests, saving an estimated ₹1,100 crore in out-of-pocket expenses for patients.
• Supply issues, such as reagent shortages, are marring the programme.
Labs Issues
• Lab representatives in Kerala argue that the space and educational requirements under the Kerala State Clinical Establishments Act are unviable.
• The state government does not recognize paramedical degrees/diplomas, requiring a two-year MLT Diploma/BSc MLT or MSc MLT conducted by medical colleges or other government approved agencies.
• Space constraints are also a problem in Tamil Nadu, with amendments to the Tamil Nadu Clinical Establishments (Regulations) Rules, 2018, stipulating minimum space for sample collection for clinical laboratories.
Regulations for Standardization
• The Karnataka Chapter of the Indian Association of Pathologists and Microbiologists (KCIAPM) is asking for the strengthening of the Karnataka Act, including licensing criteria, accreditation mandates, and penalties for non-compliance.
• Mandatory SOPs for sample collection, testing, and reporting should be put in place to minimize errors.

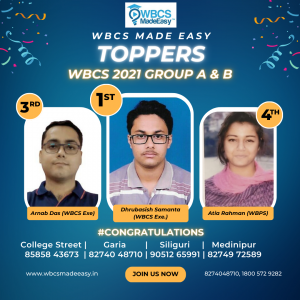
 +919674493673
+919674493673  mailus@wbcsmadeeasy.in
mailus@wbcsmadeeasy.in